8th Week of Embryonic Development Dental Lining Continues to Thicken
8 Tooth development
- Overview
- Crown development
- Initiation stage
- Bud stage
- Cap stage
- Bell stage
- Crown stage
- Root development
- Root dentin formation
- Cementum & pulp formation
- Periodontal ligament
- Alveolar bone
- Tooth eruption
- Clinical applications
Overview of tooth formation
In this chapter we cover major concepts in tooth development, saving many details for later chapters. The first big concept is the timing: so far everything has been measured in weeks, but in this chapter we measure time in weeks, months and years. Both the primary and succedaneous teeth begin developing early in embryonic development—around week 5. To put this in perspective, that is only shortly after the mouth forms– the ruptures in week 4. The process of tooth development begins around week 5. When tooth development ends is more complicated, as listed in Table 8.1 (note: any timeline you see most likely reports an average or most common age, there is significant variation in the timeline between individuals).
| Tissue: | Develops during: |
|---|---|
| crown enamel and dentin – primary | embryonic week 5 to 8 |
| crown enamel and dentin – succedaneous | embryonic week 8 to after birth (5 years) |
| root dentin and cementum – primary | embryonic to after birth (1 – 3 years) |
| root dentin and cementum- succedaneous | after birth (6 – 25 years) |
| , alveolar bone, ← | tooth eruption |
The next big concept is the importance of the very first stage (, or ). Small regions of epithelial cells in the are induced to speed up ←. This happens because of secretion of ← from ← below. You can't see this under the microscope (not without more specialized tools than the stain). As a result, this early phase is often skipped in histology books. That is a shame, because getting the correct number of teeth to form requires complex communication. Not only do the correct number need to form, the spacing between succedaneous teeth depends on where primary teeth develop. To put that another way, the embryo is making plans 5 weeks after fertilization for events that happen 5 to 10 years later. To put it yet another way, when the embryo is about 1.5 mm in length (about 1/16th of an inch), it is making plans for the spacing of teeth in an adult skull that will be 150 mm across (about 6 inches). We think this early communication is really cool. There are, however, more names associated with later stages (usually named after long-dead European men), and those names appear on licensing exams, so we cover those in detail as well. Lucky you.
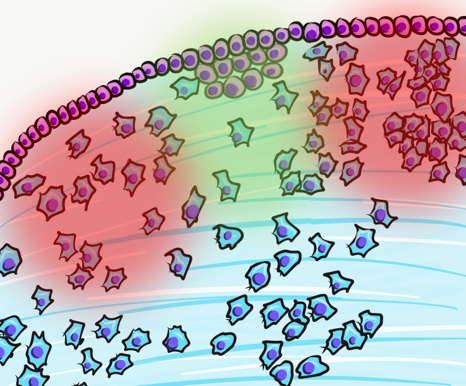
The third big concept is the of the different parts of a tooth and periodontium. Enamel is produced by cells derived from the , whereas dentin, cementum, pulp, and alveolar bone are derived from . While the hard tissues enamel, dentin and cementum share physical characteristics with ←, enamel has notable differences because of its different lineage. Perhaps the biggest difference is that people cannot grow new enamel after teeth erupt. Enamel can passively re-mineralize under the right conditions, but this does not involve the activity of human cells, ← or enzymes (which are more efficient). The enamel-producing cells, including the scaffolds and enzymes they secrete, are lost during tooth eruption. In contrast, dentin, pulp, cementum and the contain cells throughout the life of a tooth, and have a much higher capacity to undergo and following trauma.
The fourth big concept is that the ← is worthy of attention. We did not say (one of the three ), but mesenchyme (the tissue type)—the difference is important. Most mesenchyme is derived from mesoderm, but tooth connective tissues are derived from ← plus mesoderm. We give this mesenchyme a unique name: . This leads to similarities in the behavior of tooth and brain cells, which makes less sense to people who haven't learned embryology.
The fifth big concept is that enamel and dentin-producing cells do not form separately. They induce one another in a fashion. After their team-effort, the cells move apart from one another and do their own thing. This reduces the chances that enamel or dentin will be produced in the wrong place or wrong time. Production of these tissues requires a special set of conditions, one that occurs only briefly during early embryonic . Unfortunately, this makes it harder for medical professionals to re-create these conditions later in life should enamel or dentin production be beneficial.
The sixth and final big concept is that the process of tooth eruption is complicated. There are multiple steps which are poorly understood, and scientists disagree on which steps are important. We cover what is known, but we can let the experts keep arguing. What is important to us is that to learn about the of the , alveolar bone and ←, we must cover tooth eruption. Tooth eruption should be considered a developmental process even though it happens long after the embryonic and fetal stages.
Crown development
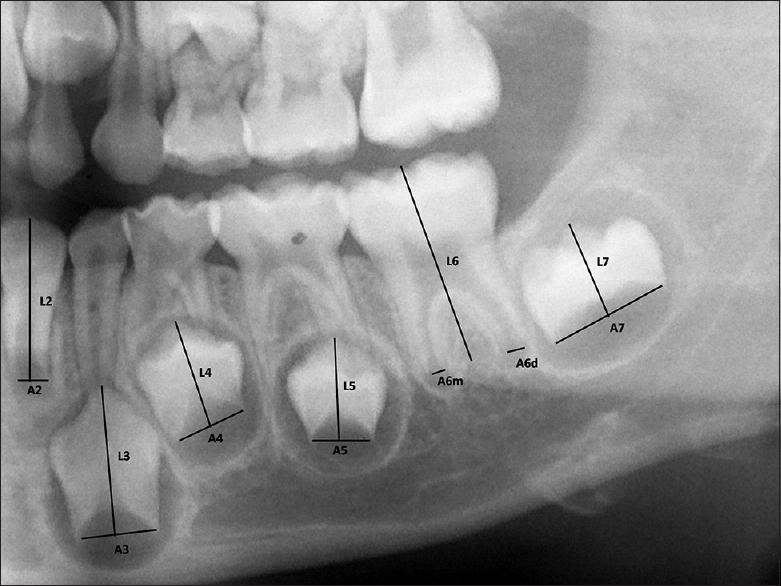
"Cameriere's method of measurement for the teeth with open apices" by Navaneetha Cugati, Ramesh Kumaresan, Balamanikanda Srinivasan, Priyadarshini Karthikeyan is licensed under CC BY-NC 3.0Tooth formation, or , starts with primary teeth around weeks 5 to 6, and succedaneous teeth around weeks 9 to 10. Odontogenesis is similar to ←, teeth arise from of epithelium, derived from . Hair follicles share this pattern as well, but instead of being called a tooth follicle, teeth grow from . At week 5, the oral cavity is lined by ectoderm-derived epithelium, and deep to that is ←. For the skin and most of the oral cavity, the layer of mesenchyme is derived from . Teeth, however, grow from ridges called the , found on the and the , along the occlusal border. Here, mesenchyme contains clusters of ← that migrated from the . Hence, we say the connective tissues of the teeth are derived from (or ecto-mesenchyme). Remember, because neural crest cells come from the neural tube, and the neural tube invaginates from the ectoderm, these cells are ectodermal by lineage. They go through an ← and resemble mesenchyme derived from mesoderm under the microscope. If you remember how cells express enzymes during this transition, you shouldn't be surprised to see these enzymes re-used during , and re-used yet again during .
By 8 weeks (before the palate ), there are 10 in each (the regions fated to become the maxillary and mandibular alveolar ridges). The tooth buds of succedaneous teeth begin forming around this time, before the primary buds have made any enamel or dentin. Both primary and permanent buds develop into crowns and become surrounded by the maxilla and mandible (Fig. 8.2).
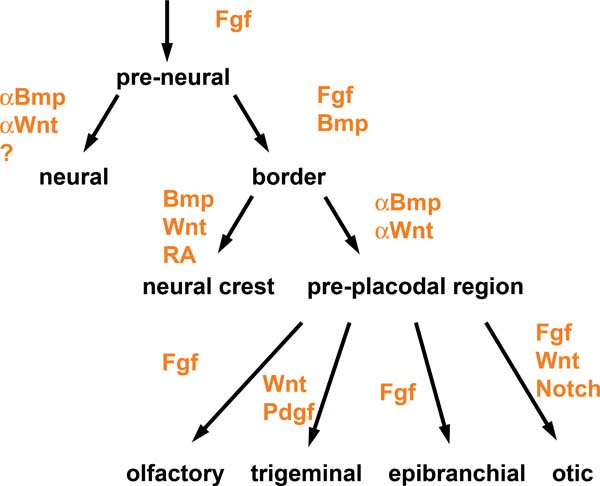
"Signaling pathways in placode formation" by Andrea Streit, Stembook.org is licensed CC BY 3.0Induction (or initiation)
The first step is poorly understood. coordinate with one another through ← signals to the correct number of , at the correct distance apart from one another. Neuro-mesenchymal stem cells secrete a number of ← forming complex gradients. Overlying responds to the morphogen gradients.
Two important ← in tooth development are members of the and the families of signaling molecules. There are more signals involved, which is illustrated in Fig. 8.3 (further reading). As you might guess from their full names, BMP and FGF aren't unique to tooth formation. These two morphogens different cells to do different things at different times and locations. At this time and location, they induce to ← into instead of . Other morphogens inhibit tooth bud induction, ensuring proper spacing is established. One of the first visible responses in the ectoderm is — certain regions begin to grow thicker, called tooth . Not every book (or exam) includes placode as its own stage, be aware. Furthermore, placodes may be called the or may be listed as a part of the dental lamina—fate mapping experiments can't easily be done on humans to determine which is more correct. The important concept is most of the oral mucosa described in chapter 3 is derived from ectoderm and , while the teeth and periodontium are derived from ectoderm and the of a tooth bud.
Bud stage
Continued of the allows us to see the next stage of tooth development under the microscope more easily, the . The name bud comes from the fact that tooth buds look like leaf buds on a plant. In the spring, you can see where leaves are to grow on plants by the location of leaf buds. Leaf buds are not leaves yet, just bumps. Tooth buds begin to appear around week 6, and ultimately 10 tooth buds form on the and . In addition to proliferation of ectodermal cells, also proliferate. This makes the ← in a tooth bud appear denser than the mesenchyme in nearby regions that form the of the . Those regions have more of the ← and fewer cells.
Enamel organ" by Dozenist is licensed under CC BY-SA 3.0 Cap stage
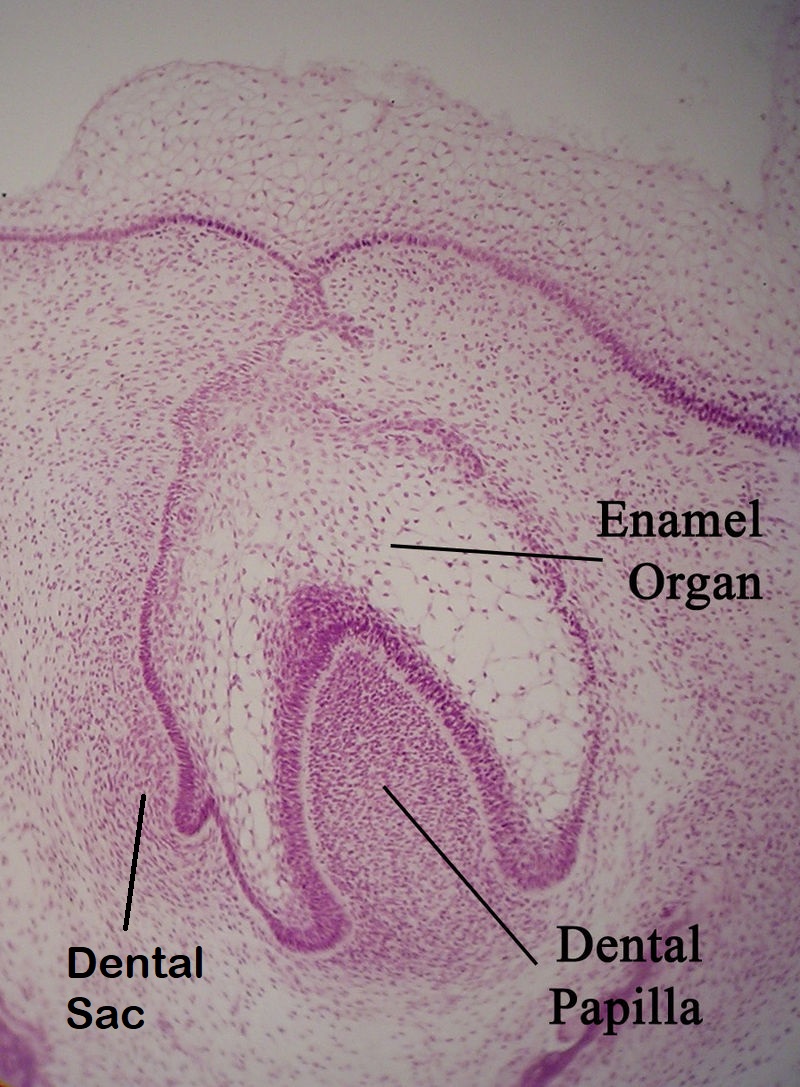
Around week 10, the continues to and it bumps into the cluster of below. This cluster of neuro-mesenchymal stem cells is called the . The dental papilla forces the ectoderm of the to grow around it. As this happens, the ectoderm resembles a hat, hence the name . At this time, the has two prominent parts—an inner and an outer layer. The epithelial cells near the dental papilla are referred to as the , because some of them ← into cells that produce enamel. Below the dental lamina, the of the forms dentin and pulp. The neuro-mesenchyme on the outside of the dental lamina is called the (or dental follicle), which forms cementum, and alveolar bone. All three together—the enamel organ, dental papilla and dental sac—are collectively called .
At this time, the process repeats (or ). Cells of the on the lingual side of the cap are induced to form another , and the succedaneous teeth bud off the developing primary . Imagine taking Fig 8.5, rotate it 90o, superimpose that onto the , and you have succedaneous formation. Exceptions to this include the 2nd and 3rd molars, which do not succeed primary teeth. Their tooth buds develop from similar to the primary dentition. Furthermore, the tooth germ of succedaneous teeth can move as they develop— does not always occur from the lingual side. For instance, the maxillary incisors generally erupt from the facial direction.
Bell stage
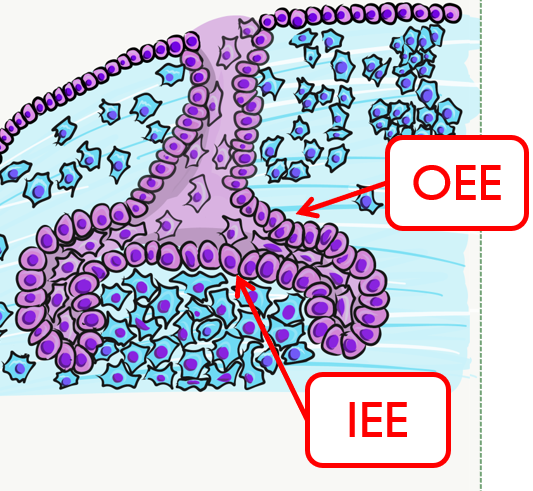
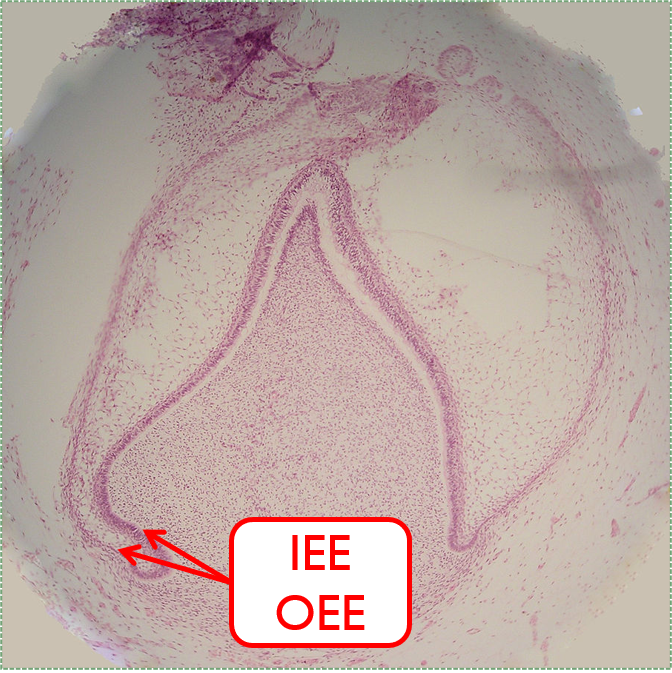
By the 11th or 12th week, and continue to . As the epithelial cap becomes larger, it resembles more of a bell shape, hence the name . Hats worn by people are usually smaller than bells on clock towers, which may help you remember which stage comes before the other. At this time, the contains two layers of cuboidal cells named the inner enamel epithelium () and the outer enamel epithelium (). The IEE is next to the , with a basement membrane physically separating the two. The IEE ← into and produce enamel, while the OEE is involved in and forms the ← that bridges the tooth surface and .
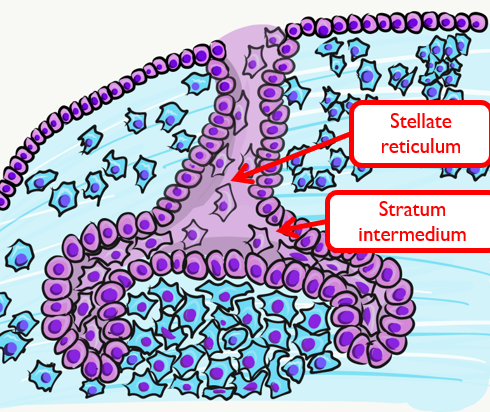
Two additional regions of the develop at this time. The is on the opposite side of the from the . These cells work with the IEE to form enamel. Past the stratum intermedium are ectodermal cells called , named for their star-shaped rather than cuboidal appearance. These cells help the IEE to ← and begin enamel production. These cells are found in the superficial but not the deeper regions of the growing , which is why enamel is only produced in crowns and not in roots of teeth.
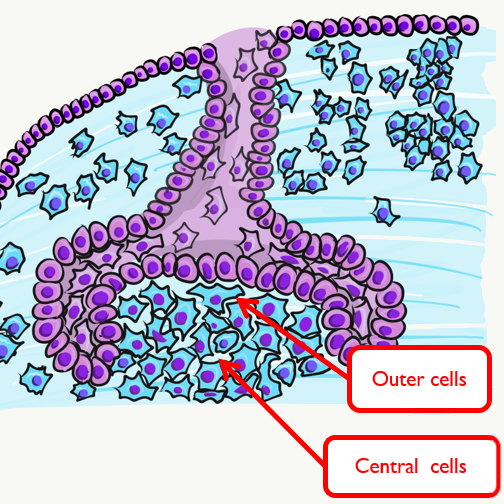
The may be subdivided at this time into an outer region and a central region. The outer cells ← into , while the central cells form many cell types found in pulp. It is worth noting that cells are not or odontoblasts at this time. These cells are epithelial and . Based on their relative location, we know what they are to become in the near future, assuming they receive the correct ←.
A brief overview of the formation of ameloblasts and odontoblasts
During the , interactions between the , and outer cells of the the ← of and . First, the that physically separated the IEE from the of the dental papillae disintegrates. The IEE contacts made by neuro-mesenchymal stems cells, am=nd they differentiate into . The prefix pre- indicates that differentiation is not considered complete at this time. The IEE looks different: cells elongate, changing from a ← to a ←. Pre-ameloblasts then produce ← that induce neighboring neuro-mesenchymal cells to differentiate into (the cells that make dentin). Newly formed odontoblasts begin producing a squishy immature form of dentin (). Molecules in pre-dentin signal back to the pre-ameloblasts. Morphogens from the also signal to pre-ameloblasts. The combination of these 2 signals induces the differentiation of pre-ameloblasts into (the cells that make enamel).
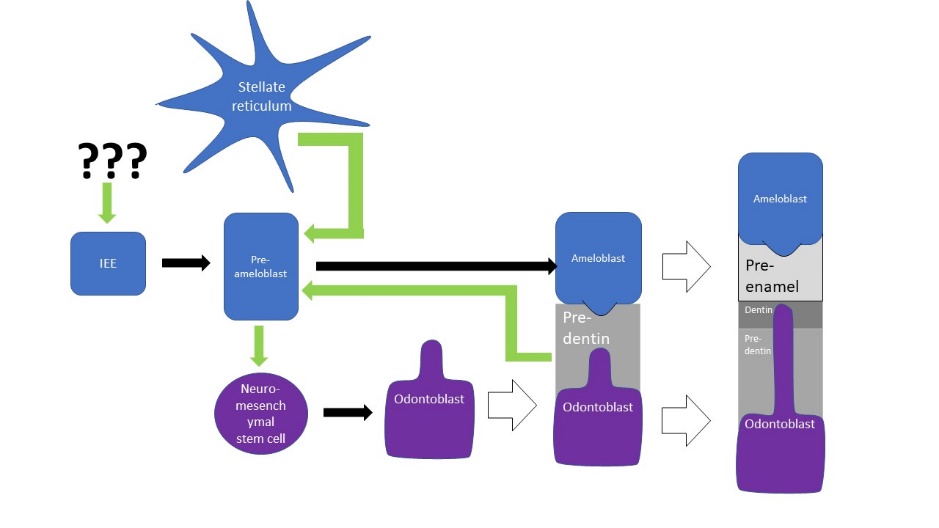
This is a common pattern in developmental biology. A dual effort is known as reciprocal induction. This is significant because it makes it hard to re-create one type of cell later in life (such as an ) without also re-creating its partner (in this case, an ). Furthermore, one must also re-create the conditions these cells were in during reciprocal induction (in this case, being close to ).
, the formation of dentin, therefore begins before , the formation of enamel. This results in dentin being thicker than enamel. As secrete , their cell bodies are pushed deeper, but they leave a log tube-like extension called the within the pre-dentin. By the time a tooth is done growing, the odontoblastic processes extend through nearly the entire layer of mature dentin. , on the other hand, do not grow an extension. There is a little bump on each ameloblast facing the enamel, and this bump is called . There is important clinical significance related to odontoblastic processes coming up in subsequent chapters. Tomes' process, on the other hand, is a name of a bump histologists use to identify ameloblasts during embryonic development (and a name prospective dental hygienists get asked about on license exams).
Crown stage
The second half of the is the late bell stage, or the . During this time the crowns of teeth form by the secretion of molecules by and . No new cells of these types form, teeth continue to grow by the addition of . Because the ECM mineralizes and hardens, these tissues must be added . This is somewhat similar to the growth of ←, only the enamel and dentin-producing cells do not get trapped between layers of hard tissue. Instead, these cells migrate in a direction (relative to the cell) as they secrete matrix. Its important to note the process of crown formation finishes before mineralization of the mandible and maxilla, but mineralization of the crowns takes more time, finishing within the first year or two of life. The timeline for succedaneous teeth is more variable (a timetable may be found on wikipedia).
Root Development
Latebellstage11-18-05 " by Dozenist is licensed under CC BY 3.0 / Iabels added The cervical loop and HERS
We must jump ahead in time to cover root development: months for primary teeth, and years for succedaneous teeth. After the crown stage, the leading edge of the and continue to grow around the . However, they are not separated by . Together they are called the . As the cervical loop continues to grow deeper, it is called Hertwig's Epithelial Root Sheath (). The pattern of HERS growth determines the shape of the root(s). This is similar to a cake mold: HERS does not become the roots, it guide their shape. HERS does not grow evenly around the dental papillae of larger teeth. Instead, HERS grows faster in some regions as it extends over the dental papilla, perhaps the way chocolate fudge drips over a ball of ice-cream unevenly. On larger teeth, this produces multiple roots. The cervical loop forms early in embryonic development, but HERS continues to grow after birth. The roots wont completely mineralize until years after .
Cementum formation
contains and , but no . This leads to key differences between the crown and roots of teeth. The IEE induce the formation of in the roots just as it did in the crown, but when odontoblasts form , the lack of a signal from stellate reticulum means the ← of does not occur. Hence, roots do not contain enamel. Instead, most of the IEE and OEE cells undergo ←. A few are left behind, which get the name the (ERM). These leftover cells may have functions in the of damaged root tissues, although this is not currently well understood.
After the majority of the epithelial cells are removed, of the contact . Getting closer to secreted by them to ← into . Cementoblasts then cover the root dentin in a relatively thin layer of cementum. At first, the cementum produced is pure ECM. Because it lacks cells it is called . Later, in the apical root regions, cementoblasts become trapped within the they secrete. This is . The cells are called once trapped within . The presence or absence of cells is easy to identify under the microscope. However, it is the polarity of ← fibers in the ECM that is more important clinically. This will be covered in Chapter 11.
Tooth eruption
We now jump forward in time yet again. Even though process of happens long after embryological , it should be considered a developmental process. Another way to say that is the teeth continue to undergo after birth. Because this process involves cells of the and , we discuss it here.
After the roots develop, of the that did not come into contact with ← into and . These form the and . The PDL anchors to cementum first, then to alveolar bone after eruption. Therefore, development of the PDL occurs during tooth eruption, much later than the formation of dentin and enamel.
First, the force or forces that cause teeth to erupt are not agreed upon. It is not even clear if it is a pushing or a pulling force, or a combination of the two. Whatever the cause or causes of tooth eruption are, movement of the crowns into the oral cavity is known as . One might imagine that as a root grows deeper and bumps into the edge of a bony socket, further lengthening of the root would force the crown upwards. This would be similar to jumping: with your legs bent and feet on a hard floor, rapid extension of your legs pushes you upwards. This is known as the root formation theory. To say this causes tooth eruption, it has to be both necessary and sufficient (a phrase commonly used in biological research). Because root-less teeth can erupt suggests root growth is not necessary for eruption.
We are going to use the terms necessary and sufficient a few more times. Before we do, here is a simpler scenario: after you stop your car at a red light, to get the car moving again requires taking a foot off the brake, applying a foot to the gas pedal and having gas in the gas tank. All three are necessary, but none of them is sufficient to move your car through the intersection.
We know bone is necessary. Bone remodeling involves coordinated activity between and (the ). However, tooth eruption is a different than the dynamic equilibrium of bone tissue. During tooth eruption, both osteoclasts and osteoblasts are active. However, they do not work togther as part of the , instead they work at different locations. As a result, equilibrium is not maintained. Bone tissue is removed above the tooth, but added below the tooth. We covered evidence for this when we discussed how permanent teeth fail to erupt in people with ←. There, a faulty enzyme lead to the inability to degrade proteins, leaving permanent teeth trapped within their bony crypt. This suggests bone remodeling is necessary, but not necessarily sufficient.
For the primary teeth, as growing roots encounter mineralized bones tissue below, pressure is put on the cells of the . In response, the secretes ← that induce bone resorption. One morphogen is , a morphogen that induces osteoclast differentiation. Another is Parathyroid Hormone (PTH), which is called a when it is secreted into the bloodstream. Here, it is secreted into the , only stimulating activity near the enamel organ. Because stellate reticulum is at the surface of enamel, these signals induce the formation of a pathway above the tooth, allowing it to erupt.
Clearing a path is necessary for tooth eruption, but it does not cause the tooth to move. As roots grow, they put pressure on bone tissue in the alveolar sockets below. Pressure on bone tissue triggers release of which leads to the deposition of bone tissue, pushing teeth outwards. Bite forces also contribute to BMP secretion. As we mentioned earlier, root growth is not necessary, but BMP secretion is necessary. That doesn't really make sense, does it? We must be missing some critical information.
We know root growth is sufficient to induce BMP secretion, and BMP secretion is necessary for tooth eruption. However, there may be something else that can stimulate BMP secretion. That is our mising piece of critical information. Further evidence that pressure is necessary comes from observation that teeth fail to erupt in the absence of healthy . In fact, pressure created by of the PDL may trigger the to secrete ← that trigger ← as well as bone tissue to release . Fibroblasts not only secrete ←, they it as well. Shortening of collagen fibers anchored to cementum would pressure on both the tooth root and alveolar socket. So does this happen? Polarization of PDL fibroblasts is observed before tooth eruption, suggesting that remodeling of PDL collagen fibers inserted in cementum may actively pull the tooth outwards. It is currently unknown whether this involves ← morphogens, signals which have been well established in their role in polarizing epithelial cells. It seems possible, given the of PDL fibroblasts: (which means , the same lineage as highly polarized and ).
But we are still left with a major question: how can the be necessary for tooth eruption if a rootless tooth can erupt? Can a rootless tooth have PDL? Lets refresh what we know about the PDL. The PDL develops from the remaining neuro-mesenchymal stem cells after receiving a signal from the . We know it is not the BMP signal that induces neuro-mesenchymal stem cells to develop into odontoblasts, cementoblasts or osteoblasts. We know the PDL first connects to cementum during eruption, and connects to alveolar bone after eruption. It seems unlikely that the PDL could develop on a rootless tooth, and even if the PDL did develop, it would have nothing to attach to. So next, let's summarize what we know about tooth eruption:
| Action | Reaction | Neccessary or sufficient for tooth eruption? |
| root growth | pushes down (against alveolar socket) | not necessary* |
| triggers BMP secretion in alveolar socket triggers PTH and RANKL secretion from stellate reticulum | necessary | |
| unknown factor(s) | ||
| PTH and RANKL secretion | clears a pathway above tooth | necessary |
| BMP secretion | bone deposited in alveolar socket | necessary |
| bone deposited in alveolar socket | pushes up (against tooth root) | necessary |
| PDL attaches to cementum | pulls tooth from above | necessary |
Now that we have summarized the facts we have, it is a good time to re-visit our troublesome assumption: teeth can erupt without roots. When professionals report the eruption of rootless teeth, do they mean these teeth never formed roots, or did the roots undergo resorption during eruption? Sadly, waiting until we see the eruption of a rootless tooth is too late to answer this question. We need time-travel, psychic abilities, or lots of radiographs of unerupted teeth. Furthremore, it is difficult to make a strong conclusion that root growth is not necessary when the original report of rootless tooth eruption is missing. No wonder the force of tooth eruption are not agreed upon. Luckily, we do not need to solve the controversy here. But it does bring up an important concept: when things don't make sense, question your assumptions! Here is a good article on how and why:
-
discussing assumptions using a gender-bias issue
Don't be disappointed if science raises two questions for every question it answers. Let's our car metaphor as we summarize what we know about tooth eruption. The best evidence at this time is that a foot must be lifted off the brake pedeal ( and PTH clear a pathway in bone tissue above), a foot must be placed on the gas pedal ( causes bone deposition in the alveolar sockets and pushes teeth from below) and there must be gasoline in the gas tank (the pulls teeth outwards).
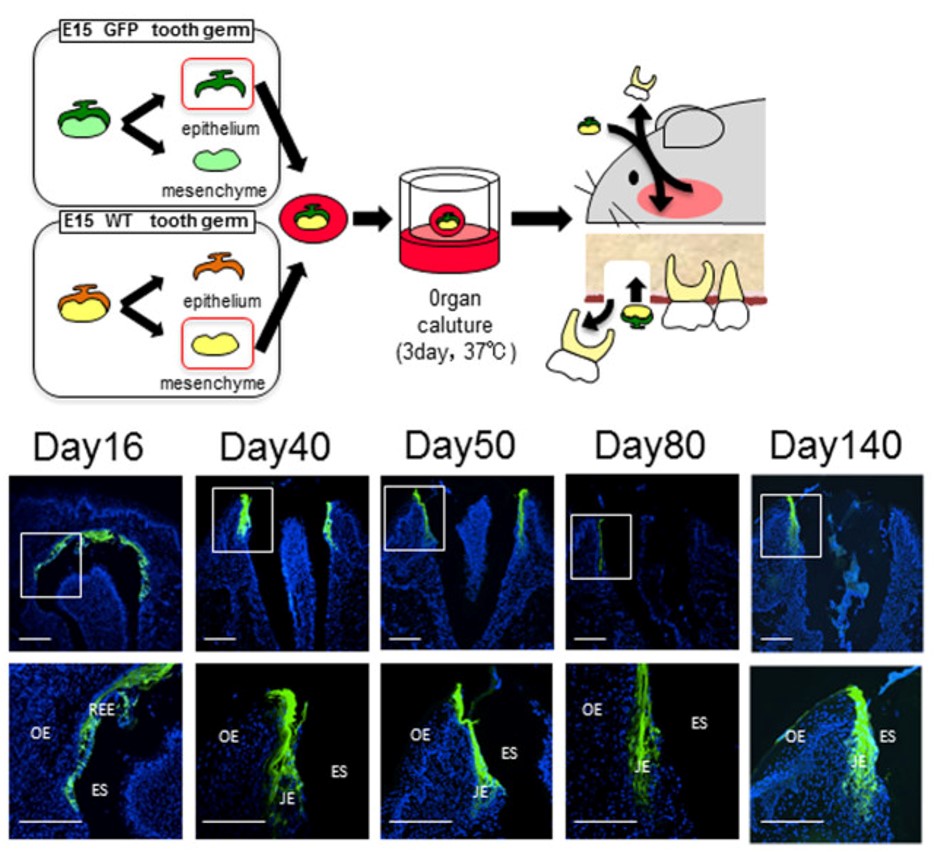
"The JE attached to the bioengineered tooth was derived from the odontogenic epithelium." by Sara Yajima-Himuro, et al is licensed under CC BY 3.0But wait, there's more. Changes in the gingiva must also occur for tooth eruption to proceed. of after is known as . Old tissue is removed to clear a path for the tooth to erupt. Teeth do not just tear their way through the gums. But do not think of this like digging a tunnel for cars to drive through. The first difference is oral mucosa is connected to the tooth near the as it erupts. Otherwise, oral bacteria could enter the and cause . The second difference is there is no tunnel. Bone tissue is added behind teeth as they erupt. So think of this like digging a lacuna for just one car, filling the lacuna behind the car as it travels, and trapping the car just as its front end clears the other side.
Before eruption begins, the crown of the tooth is topped with 2 layers of epithelial cells, and . Collectively, these two layers of epithelial cells are called the Reduced Enamel Epithelium (). Like the and separation of cells during ←, the REE becomes separated from the during . During tooth eruption, the REE re-joins the oral epithelium. As the REE it re-forms ← and pairs up ← with oral epithelial cells, but maintains contact with enamel. Many REE cells undergo ←, but those that remain become the ←. This special epithelium maintains contacts on both sides of the tissue: (enamel) and ().
Some of the may not with the nor undergo ←, and remain partially stuck to the surface of a newly erupted tooth. This is known as the (or the more old-fashioned name Nasmyth's membrane). It can easily be removed by gentle brushing or mastication.
Because in the are lost with tooth eruption, no new enamel is produced by human cells afterwards. is faster and more organized than passive re-mineralization because it involves a protein ← which catalyzes crystal formation. Furthermore, the lack of REE means that gingiva cannot form ← with ←. Understanding how junctional epithelium forms in the first place improves our ability to trick cells into behaving more like junctional epithelium.
Lastly, it is interesting to consider why only two sets of teeth erupt, making us (and most mammals) diphyodonts. The teeth of many other animals are and replaced repeatedly throughout life (polyphyodonts). Why don't tooth buds the exfoliation pattern of ? The answer is likely our oldest mamallian ancestors were tiny and did not live long. They lived long enough to benefit from replacing hair follicles seasonally (you dog owners understand). But multiple sets of teeth would not have been beneficial. So why two sets of teeth? For that, we must go back even futher in evolutionary time. The ancestors of the very first mammals one set of teeth for chewing their way out of a hard eggshell, then a second set for eating food. Apparenly, our recapitulates that . So why did we say most mammals? The teeth of elephants and manatees grow very differently from our own. Their teeth erupt from the distal end of the jaws and pushing older teeth mesially, not twice but repeatedly throughout their lifetime. Should we study elephants and manatees to see if we can repeat this in humans? That is up to you, but time is running out.
Summary of dental tissues
| enamel | dentin | pulp | cementum | PDL | alveolar bone | |
|---|---|---|---|---|---|---|
| produced from | enamel organ | dental papilla | dental papilla | dental sac | dental sac | dental sac |
| lineage | ectoderm | neuro-mesenchyme | neuro-mesenchyme | neuro-mesenchyme | neuro-mesenchyme | neuro-mesenchyme |
| tissue type | epithelial | connective | connective | connective | connective | connective |
| formative cells | ameloblasts | odontoblasts | fibroblasts | cementoblasts | fibroblasts | osteoblasts |
| cells in mature tissue | (odontoblastic processes ) | odontoblasts fibroblasts NMSCs | cementocytes | fibroblasts cemetoblasts osteoblasts PDLSCs | osteocytes | |
| resorptive cells | odontoclasts | cementoclasts | osteoclasts | |||
| resorptive cell activity | exfoliation | exfoliation | throughout life, changes during eruption and exfoliation | |||
| Mineral% | 96% | 70% | 50% | 66% | ||
| Organic & water% | 1% protein 3% water | 20% protein 10% water | 38% protein 12% water | 21% protein 12% water | ||
| major protein(s) | amelogenin enamelin | collagen | collagen fibronectin | collagen | collagen | collagen |
| Forms during | embryonic | embryonic (crown) post-natal (roots) | embryonic (crown) post-natal (roots) | post-natal (roots) | tooth eruption | tooth eruption |
| Vascularity | vascular | vascular | vascular |
Clinical considerations
Induction stage complications
Problems with the of leads to the formation of too few or too many teeth.

"Incontinentia pigmenti presenting as hypodontia in a 3-year-old girl: a case report" By Kitakawa et al, Journal of Medical Case Reports 2009, is licensed CC BY 2.0Anodontia
Failure during the stage results in missing teeth, or . This may include inadequate release of ← by , mutations in the morphogen proteins, or that interfere with activation of ←. Partial anodontia (also called ), where one or a few teeth are missing, is most common. The most commonly missing teeth are permanent maxillary lateral incisors, 3rd molars, and mandibular 2nd pre-molars.

"Ectodermal dysplasia ", by Pratheeba227 – photographed at Govt Vellore Medical College, is licensed CC BY SA 3.0Ectodermal dysplasia (part 2 of 2)
← is covered in chapter 6 where we discuss the of ←. When signals from ← are reduced, regions of that are supposed to grow faster than others do not get the boost in growth they need. This includes , finger and toenails, , sweat glands and salivary glands. This may cause some or all of these structures to not develop at all (for teeth, ), to develop in reduced number (for teeth, ), or reduced in size (for teeth, ).
For those who cannot afford or are too young for ←, complete or partial anodontia may be visible, as well as microdontia (Fig. 8.16). Children do not receive dental implants because implants do not grow in size to match a growing jawline. Multiple sets of dentures are an option (again, for those who can afford the treatment). Now is a good time to double-check you can distinguish between and . If you haven't had Latin or a good medical terminology class, remember a hypo-dermic needle goes lower than the dermis, while micro-biology is the study of small stuff.

"Fig. 5"by Toby Hughes et al., J. Dental Anthropology is licensed under CC BY 4.0Hyperdontia
, the formation of extra (supernumerary) teeth, occurs when of occurs where it shouldn't. This is often a genetic condition. The most common extra teeth are between the central incisors (), distal to the maxillary 3rd molar (4th molar, or ) and the premolar region of either dental arch ().
Bud and cap stage complications
Problems in the of tooth development may lead to teeth that are too large () or too small (). This may affect all the teeth, some teeth, or a single tooth.

"Periapical radiography of superior central incisive permanent geminated" by Katia Simone Alves dos Santos et al., Intl J Morphology is licensed under CC BY 4.0Gemination
Tooth (twinning, as in the constellation Gemini) occurs when a single is partially divided in two. This may occur if the growing tooth germ bumps into a small dense region in the dental arch. Under healthy conditions, teeth grow within loose ← tissue, which later ← into osseous tissue and calcifies. A geminated tooth, coming from a single tooth germ, is larger than average, but has a single pulp cavity, hence this patient has an instance of (but not ).

"milk.teeth.fusion" by Sarefo is licensed under CC BY-SA 3.0Fusion
(joining) of two into a single germ can also cause a larger-than-average tooth to develop. In this case, is accompanied by . The fused tooth has two separate pulp cavities. This occurs when of two tooth germs occurs close to one another, or when external pressure forces two tooth germs closer together. Tooth germs can fuse during early stages of tooth development because the tooth germ is soft epithelial and ← tissues. Getting too close together during later stages, when enamel and dentin are calcified, leads to plain-old tooth crowding (malocclusion).
It is worth a mention that the fusion of teeth involves two separate buds growing into one large structure when their secretions meet. Syndactyly, the fusion of toes or fingers, is not really a fusion but a lack of separation due to diminished or absent ← signals.
"Radiographic view of Teeth" by Eduardo Borie E, et al, Intl J Morphology is licensed under CC BY 4.0Dens in dente
(tooth within a tooth, or dens invaginitus) occurs when a small region of the grows too fast and a second time, into the , during the . This sub-region of the enamel organ continues to develop like a smaller version of the original enamel organ, creating what looks like a miniature tooth within the main tooth. This can complicate a root canal surgery, but otherwise only makes for interesting radiographs.
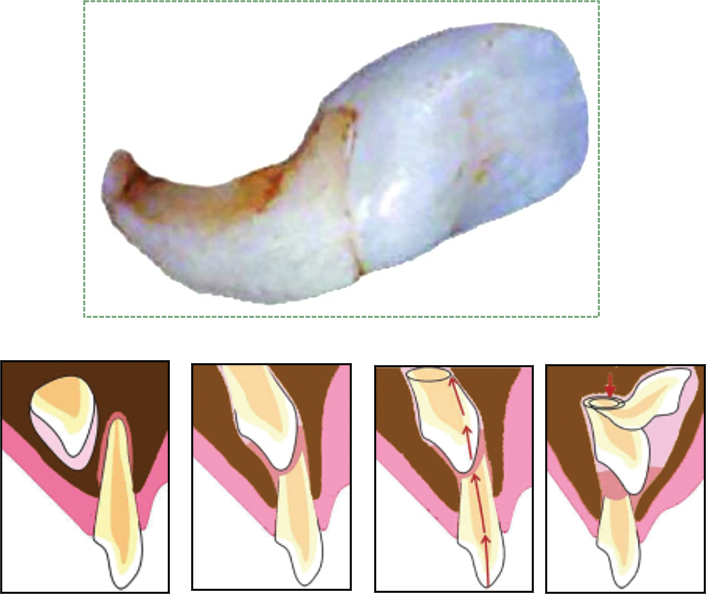
"Figs 1-5" by Pawanjit Singh Walia, Intl J Clinical Ped Dentistry is licensed under CC BY 3.0Dilaceration
, or a bend in the shape of a tooth, occurs when there is an impediment to the growth of . A delay in can cause dilaceration. This can occur because the crowns develop and calcify first, and the roots develop later. If a developing tooth bumps into calcifying osseous tissue and is forced to change its direction of growth, the older calcified part of the tooth (the crown) will have grown at a different angle from the newer, softer root(s). Alternatively, trauma to a deciduous tooth can be transferred to the deeper succedaneous tooth, causing dilaceration of the succedaneous tooth (Fig 8.21).
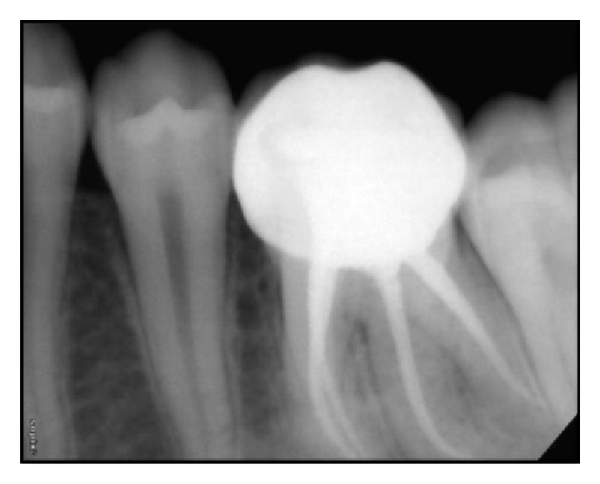
"Postoperative IOPA of 36 and 46." by Muktishree Mahendra et al, Case Reports in Dentistry is licensed under CC BY 3.0Supernumerary roots
Teeth may develop extra, or . As with , this may complicate root canal surgery, but otherwise has limited clinical significance. When the shape of the tooth is altered but no pathology results, clinicians may note there is an alteration to the of the tooth.
Eruption complications

"Own work" By Daniel Schwen – is licensed under CC BY-SA 4.0Teething
During , several tissues undergo significant remodeling, including the , and ←. This involves removal of by the secretion of digestive enzymes, and removal of cells by ←. However, enzymes aren't smart enough to remove only ECM, they tend to kill cells as well. For instance, when the secretes to clear a path for the erupting tooth, this triggers inflammation as proteins are destroyed along with ECM, leading to cell death. Inflammation can cause discomfort, tenderness or in the affected area.
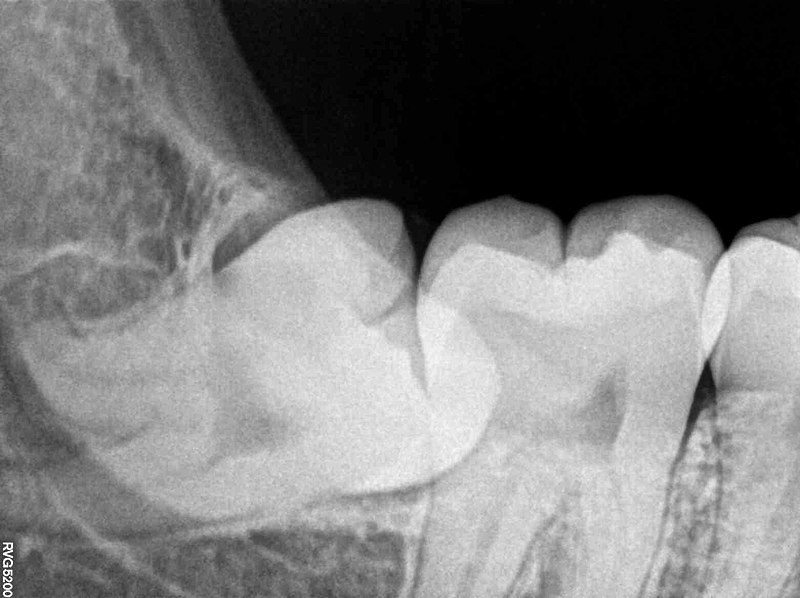
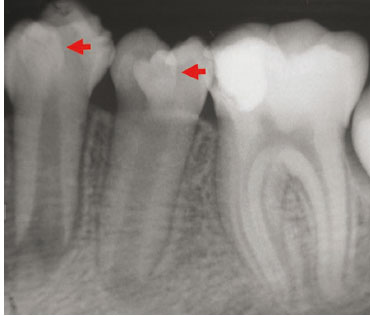
"Impacted Wisdom Tooth aka Lower Right Third Molar 48 RVG IOPA Xray" by Nizil Shah is licensed under CC BY-SA 4.0Primary failure of eruption
Primary failure of eruption () is the partial or complete failure of a tooth to erupt (otherwise known as an impacted tooth) despite a healthy eruption pathway. While there are likely many causes of PFE, one major heritable cause is a mutation that disrupts parathyroid hormone signaling from the to tissue. Parathyroid hormone activates and inhibits osteoblasts, therefore inhibiting parathyroid hormone signals leads to increased bone deposition. This leads to of the tooth prior to eruption. It also makes tooth extraction difficult or impossible, especially as time progresses. Impacted teeth may cause inflammation and pain, or may not be detected until an x-ray is performed. The 3rd molars are the most commonly impacted teeth. Complications include crowding of neighboring teeth, infection, malocclusion, and– rarely– neoplasia, making extraction an important option.
Mechanical failure of eruption
A tooth may also become impacted after erupting partially because of ankylosis of the tooth, which is termed mechanical failure of eruption (— it seems odd that it is not secondary). In contrast to , there is a physical barrier to the eruption pathway. Absence of the indicates and can indicate MFE. With MFE, orthodontic or other therapies may allow the impacted tooth to erupt eliminating the need for extraction and replacement.

"Jaw cyst" By: Coronation Dental Specialty is licensed under CC BY 3.0Dentigerous cyst
An impacted tooth can produce a cyst around the crown, called a . As the motionless tooth attempts to digest its way through , fluid accumulates between the crown and . The cyst may continue to grow in size, causing pain and trauma to the jaw bone (usually the mandible). Extraction of the impacted tooth will solve the issue. Orthodontic facilitation of may be an option as well. Rarely, the REE in a dentigerous cyst develops into a benign tumor known as an ameloblastoma. The main risk of this cancer is that similar to that of the cyst—it can cause pressure which may cause bones to break or to grow malformed. The reason this tumor is rare is that the REE cells are (non-mitotic). Furthermore, because these epithelial cells are anchored to one another by ←, this type of tumor rarely metastasizes.

"Own work" by West Exchange is licensed under CC BY 3.0Bohn's nodules and Epstein pearls
are masses of trapped in the gingiva. They may be referred to as epithelial rests of Serres in older texts, and are also called when they are located within . Bohn's nodules are produced by the , while Epstein pearls are produced by . Furthermore, remnants of can be called Bohn' nodules as well, despite lacking keratin. Their presence along the alveolar ridge may cause parents to mistake them for erupting teeth. They occur more commonly along the maxillary ridge. Bohn's nodules and Epstein pearls are transient—they go away on their own, usually within 3 months, and produce few if any disturbances.
Lastly, if you are interested in the history of embryology and long-dead European men, we offer the following. Antoine Étienne Serres collaborated with the embryologist Johann Friedrich Meckel, who named the cartilage in the that develops into the mandible (). Together, they attempted to unify embryology and the of different species (later called evolution by heritable selection by Charles Darwin and the less-well-known work of Alfred Russel Wallace). Serres' and Meckel's theory was developed further by Ernst Haeckel, who coined the memorable phrase " ," which we have quoted several times in this text.
< Chapter 7 * navigation * Chapter 9 >
Chapter review questions
harringtonallin1999.blogspot.com
Source: https://openoregon.pressbooks.pub/histologyandembryology/chapter/chapter-8-tooth-development/
0 Response to "8th Week of Embryonic Development Dental Lining Continues to Thicken"
Post a Comment